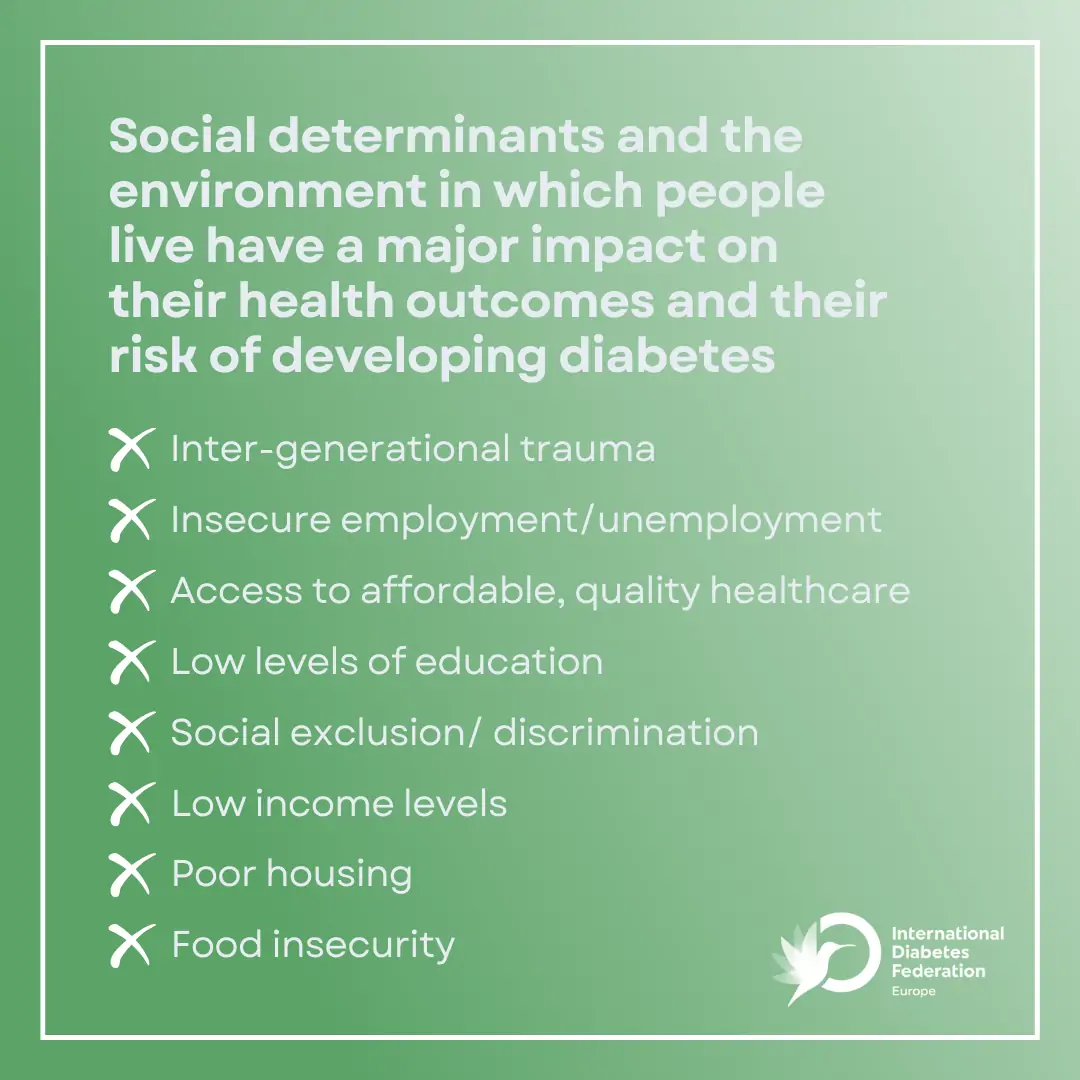
Social determinants and the environment in which people live have a major impact on their health outcomes and their risk of developing diabetes
The World Health Organization (WHO) defines the social determinants of health as the conditions in which people are born, grow, live, work and age. These factors can play a stronger role than healthcare or lifestyle choices in influencing health and significantly contribute to health inequalities and disparities, which are particularly evident in the context of diabetes. Several studies show that the social determinants of health account for between 30-55% of health outcomes. The environment in which people live also strongly influences their ability to adopt health-enhancing practices and access to health services, resources as well as support systems that can help them conduct healthy lifestyles.
Social determinants such as low income, insecure employment, limited education, food insecurity, inter-generational trauma, social exclusion and poor housing are intrinsically linked to the prevalence of diabetes and play a pivotal role in shaping health outcomes for PwD. Poverty is, for example, associated not only with higher diabetes incidence but also with inequalities in access to diabetes care. Adults in poor and near-poor households have the highest rates of diabetes and low-income populations are more likely to develop the condition. There is a strong correlation between the education level and the development of type 2 diabetes (T2D) and diabetes-related complications, which increases as the level of education decreases, placing people with a lower level of education at a 2.4 times higher risk of developing the condition. Most of these factors are intertwined and play a role at all stages of life.
Understanding the profound impact of health determinants on people living with chronic conditions such as diabetes and fostering the development of health-enabling environments are key to inform primordial, primary and secondary prevention strategies that can address the societal, cultural and environmental factors influencing health.
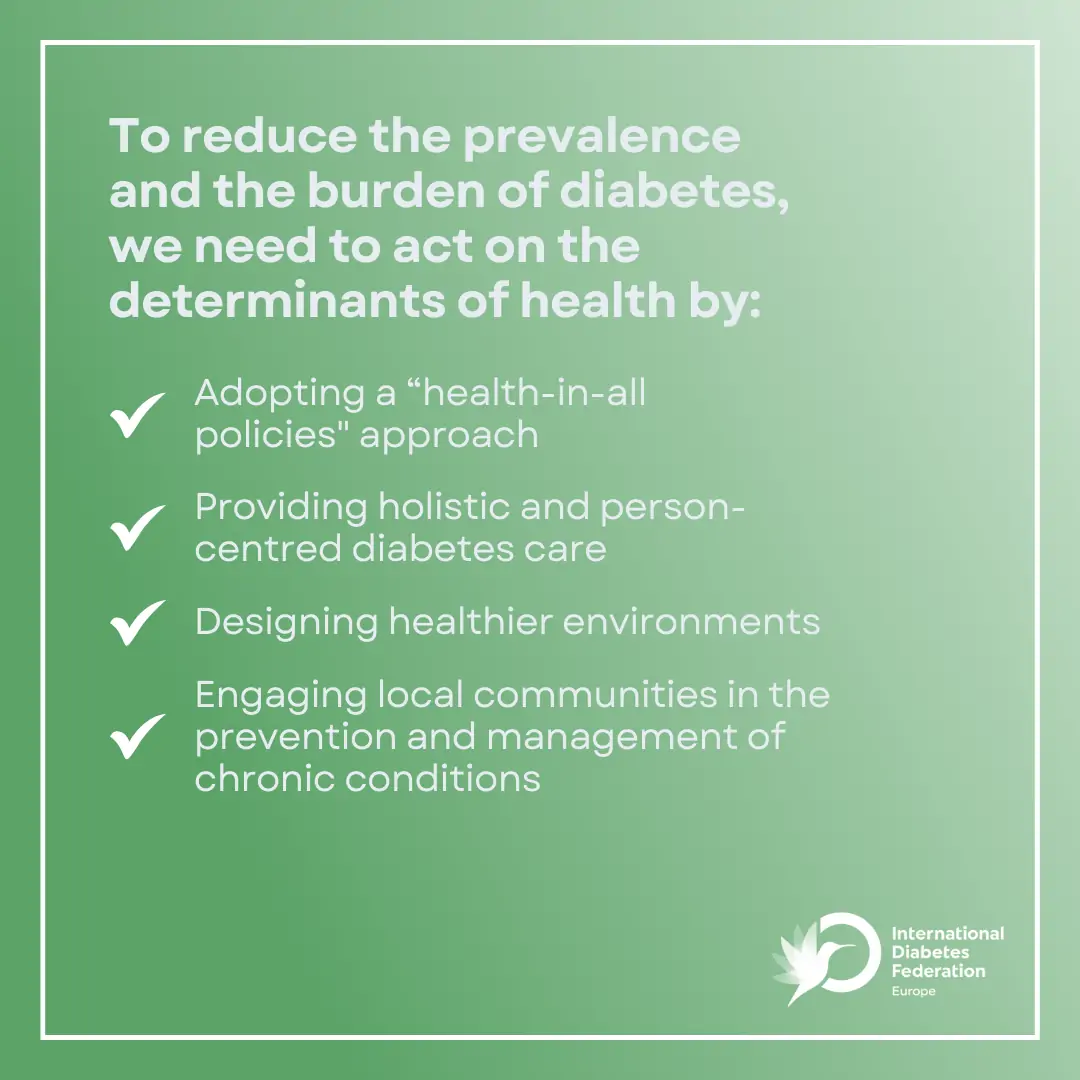
Designing healthier environments, engaging communities and providing holistic, person-centred care, can reduce inequalities among PwD and those at risk
Improving diabetes prevention, management and care requires the adoption of a holistic, person-centred approach which places the person living with the condition at the centre of their care and takes into account their specific circumstances, preferences and needs.
To tackle inequalities policy efforts and institutional responses must also focus on fostering health-enabling environments in an intersectoral and multidimensional way. This entails acting on the urban environment and the living and working conditions by considering that policies relating to food systems, labour, education, transportation, housing, etc. also have significant consequences on health. Policies should, for example, improve availability and proximity to, as well as affordability of, healthy food; integrating health-promoting approaches into urban and spatial planning; and stimulating active mobility and physical activity at local level. The active engagement of local communities through community-based interventions, which represent a cost-effective and relatable solution to support healthier lifestyles, can also play a key role in supporting people living with chronic conditions, and promoting the adoption of health-enhancing practices.
A “health-in-all-policies” approach that addresses the environmental, cultural and socio-economic determinants of health will not only benefit people living with diabetes and other NCDs, but also the general population.
In the lead up to World Diabetes Day, let’s unite to raise awareness of the need to reduce the prevalence and the burden of diabetes by acting on the determinants of health and promoting the development of health-enabling environments. Together, United, Let’s Act on Diabetes.