November 1 marks the beginning of Diabetes Awareness Month, setting the stage for the celebrations of World Diabetes Day on November 14, the world’s largest diabetes awareness campaign, reaching a global audience of more than one billion people. This year, the IDF Europe community is joining forces to raise awareness of the need to accelerate action on diabetes.
Prevention is not working well enough and health outcomes are not improving in line with innovation
Despite the incredible advances made in the prevention and management of diabetes over the past few years, the prevalence of diabetes continues to rise, health outcomes for people living with diabetes (PwD) are not improving in line with innovations and there remain many unmet medical needs for PwD. Across Europe, more than 61 million people live with diabetes and this figure is expected to reach 67 million by 2030, with one third of PwD remaining undiagnosed. This situation is placing a huge burden on individuals, societies and healthcare systems.
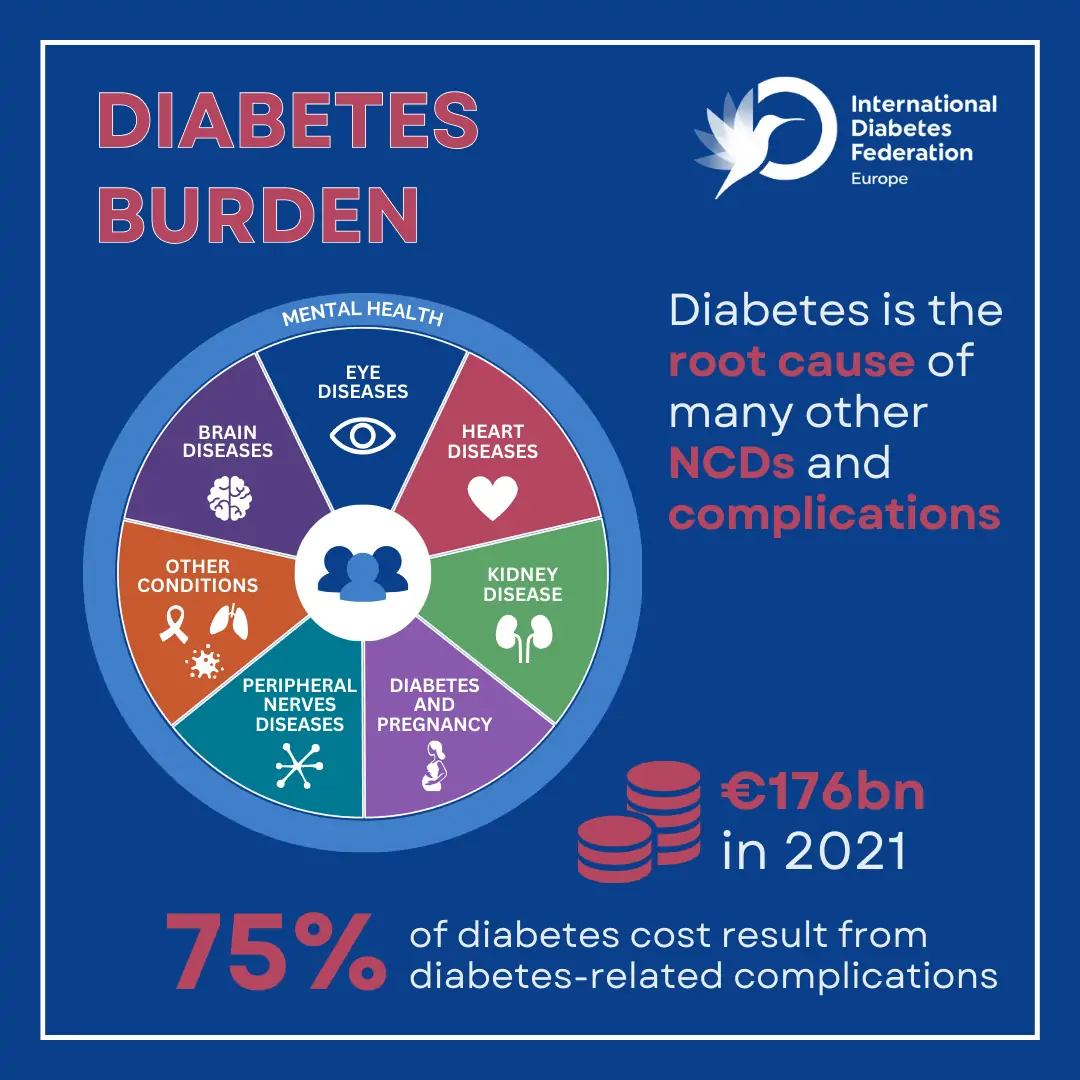
Diabetes management is hard, relentless and all-consuming. PwD and/or their relatives/carers need to manage the condition seven days a week, 24 hours a day, to prevent the development of life-altering complications which can affect every organ system in the human body. Despite strenuous management, about half the PwD do not achieve optimal blood glucose targets and many develop complications such as cardiovascular diseases (CVD) and diabetes retinopathy, which affect one third of them, and end-stage renal disease which is, in 80% of all cases, caused by diabetes and hypertension.
The burden of diabetes is also reflected in the economic loss for health systems which bear huge costs linked to an inefficient allocation of resources supporting the treatment of diabetes-related complications rather than their prevention. Some 75% of the direct European expenditure on diabetes, which stood at €176 billion in 2021, resulted from diabetes-related complications.

Inequalities persist and timely access to the adequate interventions and innovation is all too often lacking
Inequalities in access to care are also hindering the ability of PwD across Europe to optimally manage their condition and achieve the best possible quality of life. PwD need access to early diagnosis and to the right treatment at the right time, including uninterrupted access to medicines, supplies, tools and technologies, as well as the provision of self-management education and psychological support, and adequate screening for complications.
Today, researchers are paving the way for many innovative prevention, treatment and management solutions for diabetes, including major breakthroughs that could lead to the eradication of type 1 diabetes (T1D), cell replacement therapies, new sensors and long-term implantable devices for diabetes management, as well as new insulin delivery mechanisms. Nevertheless, improving the timely, equal, affordable and uninterrupted access to existing innovations is still crucial as an innovation is not successful if it is not available to everyone who needs it.
A strong political recognition of diabetes as one of the most pressing health challenges of our time, which needs to be re-affirmed in the current permacrisis era
In recent years, a growing political momentum began to reflect the urgent need to address the burden of diabetes. Several global initiatives were launched designed to improve diabetes prevention management and care, such as the WHO Global Diabetes Compact (2021), the World Health Assembly (WHA) Resolution for reducing the burden of NCDs (2021), the Global Targets for Diabetes at the 75th WHA (2022) and the new European Parliament Diabetes Resolution (2022). However, these significant policy developments have been overshadowed by the beginning of what is termed, the “permacrisis”, exemplified by the COVID-19 pandemic and other emergencies including wars and natural disasters, which are exacerbating current challenges and impeding progress in achieving better diabetes prevention and care delivery.
Reaffirming political commitments and increasing collaboration between stakeholders is therefore crucial to deliver on the objectives set by these initiatives. Strong political commitment will be key over the coming years to develop solutions adapted to the permacrisis era to improve the detection and diagnosis of diabetes as well as the quality of care and the prevention of complications, and ensure equal access to the right quality treatment at the right time and place.
No action can be successful without adequate financing and effective resource allocation
Financing and the effective allocation of resources is essential to make commitments on diabetes a reality. With 75% of diabetes costs resulting from diabetes-related complications, health systems urgently need to shift from a treatment to a prevention mindset by increasing their focus on risk reduction and person-centred, holistic and integrated care. Currently, the burden of treating complications rather than preventing them weighs not only on those living with the condition and experiencing a loss in quality of life and potentially, premature death, but also on our healthcare systems and economies. Allocating resources towards strengthening primary care would represent an investment rather than a cost. Primary care is the first line of action for the prevention and treatment of diabetes. The majority of people living with type 2 diabetes (T2D), for example, are seen at this level with primary care professionals also playing an essential role in the identification of people at risk of developing the condition, their early detection, diagnosis as well as treatment. Investing at this level would improve health outcomes and reduce the need for the costly acute and chronic care associated with the treatment of complications.
Investments in research and innovation are also essential to boost the adoption and the development of novel approaches to diabetes prevention, management and care that can address the existing unmet medical needs for PwD.
Allocating resources to the development of strong preparedness plans will also strengthen the resilience of our healthcare systems. In the context of the permacrisis, health systems should be prepared and equipped to ensure uninterrupted access for all PwD to the care they need to optimally manage their condition and prevent the development of diabetes-related complications.

Social determinants and the environment in which people live have a major impact on their health outcomes and their risk of developing diabetes
The World Health Organization (WHO) defines the social determinants of health as the conditions in which people are born, grow, live, work and age. These factors can play a stronger role than healthcare or lifestyle choices in influencing health and significantly contribute to health inequalities and disparities, which are particularly evident in the context of diabetes. Several studies show that the social determinants of health account for between 30-55% of health outcomes. The environment in which people live also strongly influences their ability to adopt health-enhancing practices and access to health services, resources as well as support systems that can help them conduct healthy lifestyles.
Social determinants such as low income, insecure employment, limited education, food insecurity, inter-generational trauma, social exclusion and poor housing are intrinsically linked to the prevalence of diabetes and play a pivotal role in shaping health outcomes for PwD. Poverty is, for example, associated not only with higher diabetes incidence but also with inequalities in access to diabetes care. Adults in poor and near-poor households have the highest rates of diabetes and low-income populations are more likely to develop the condition. There is a strong correlation between the education level and the development of type 2 diabetes (T2D) and diabetes-related complications, which increases as the level of education decreases, placing people with a lower level of education at a 2.4 times higher risk of developing the condition. Most of these factors are intertwined and play a role at all stages of life.
Understanding the profound impact of health determinants on people living with chronic conditions such as diabetes and fostering the development of health-enabling environments are key to inform primordial, primary and secondary prevention strategies that can address the societal, cultural and environmental factors influencing health.
Designing healthier environments, engaging communities and providing holistic, person-centred care, can reduce inequalities among PwD and those at risk
Improving diabetes prevention, management and care requires the adoption of a holistic, person-centred approach which places the person living with the condition at the centre of their care and takes into account their specific circumstances, preferences and needs.
To tackle inequalities policy efforts and institutional responses must also focus on fostering health-enabling environments in an intersectoral and multidimensional way. This entails acting on the urban environment and the living and working conditions by considering that policies relating to food systems, labour, education, transportation, housing, etc. also have significant consequences on health. Policies should, for example, improve availability and proximity to, as well as affordability of, healthy food; integrating health-promoting approaches into urban and spatial planning; and stimulating active mobility and physical activity at local level. The active engagement of local communities through community-based interventions, which represent a cost-effective and relatable solution to support healthier lifestyles, can also play a key role in supporting people living with chronic conditions, and promoting the adoption of health-enhancing practices.
A “health-in-all-policies” approach that addresses the environmental, cultural and socio-economic determinants of health will not only benefit people living with diabetes and other NCDs, but also the general population.
In the lead up to World Diabetes Day, let’s unite to raise awareness of the need to reduce the prevalence and the burden of diabetes by acting on the determinants of health and promoting the development of health-enabling environments. Together, United, Let’s Act on Diabetes.

Integrating care by placing PwD and their needs at the centre of their own care
According to the WHO Regional Office for Europe’s definition, integrated care entails the comprehensive delivery of quality services across the life-course, designed according to the multidimensional needs of the population and the individual and delivered by a coordinated multidisciplinary team of providers working across settings and levels of care. For a life-long and complex condition such as diabetes, integrated care is fundamental to help PwD achieve optimal health outcomes and the best possible quality of life.
Integrated care facilitates the collaboration between the wide range of care providers that are involved in the prevention, management and treatment of diabetes across all levels of care. With diabetes being the root cause of many other NCDs and complications, the integration of care is crucial for PwD who often live with, or are at risk of, developing more than one condition. This requires coordination between specialties and health services through the deployment of multidisciplinary teams and well-defined care pathways. General practitioners, endocrinologists, diabetes specialist nurses, diabetes educators, dietitians, psychologists and other specialists such as cardiologists, ophthalmologists, nephrologists and podiatrists, all play a role in diabetes care, from prevention to timely interventions that can support optimal diabetes management and prevent the development of diabetes-related complications.
The delivery of integrated care requires placing PwD at the centre of their care and understanding their needs and preferences to be able to support them in achieving optimal health outcomes. Diabetes is a life-long condition. This means that the type of support, services and resources that PwD need to manage their condition may evolve throughout their life course, from paediatric through to adult and geriatric care. Integrated and person-centred care establish personal care pathways for each PwD which are able to recognise and adapt to their changing needs and support the transition between different providers and levels of care by offering holistic and tailored support throughout their life course.
Enabling integrated care through person-centred and novel care pathways
Novel care pathways, supported by the adoption of novel technologies, protocols and the digitalisation of healthcare systems, have the potential to improve the delivery of high-quality services that enhance PwD’s quality of life by addressing barriers such as low PwD empowerment, shortages of healthcare professionals (HCPs), siloed and single-disease treatment approaches and lack of digitalisation, interoperability and IT integration.
Innovations such as telemedicine, web portals, apps, digital education services and digital therapeutics can support better care delivery in many ways while also leveraging data and the use of AI to support the deployment of more integrated and personalised care.
They can facilitate access to knowledge and information which is crucial for PwD who need to self-manage their condition 24/7 with limited input from HCPs, thereby empowering and supporting them in taking informed decisions. The need for sustained support for PwD can also be addressed by digital health models which integrate access to peer support groups. Remote monitoring/connections via digital platforms/tools, potentially removing the need for some face-to-face touch points while maintaining or increasing the frequency of contact, can also improve the quality and the effectiveness of interactions between HCPs and PwD, and subsequently free up human and financial resources for healthcare systems.
Finally, the enhanced use of big data analytics and AI can support research and innovation as well as the evaluation of healthcare interventions and the improved planning of resources while also helping to achieve better population health management and diabetes prevention. For example, population-level data can be used to identify people at high risk of developing diabetes and ensure that they receive timely and personalised care. At an individual level, improved prediction models can also support the improved prevention and management of diabetes-related complications.
In the lead up to World Diabetes Day, let’s raise awareness of the need to accelerate action towards the full adoption of integrated and novel care pathways to ensure that all PwD can achieve optimal health outcomes and the best possible quality of life. Together, United, Let’s Act on Diabetes.

Improving HCPs’ education to improve health outcomes and quality of life for PwD
Diabetes is a complex condition the management of which necessitates collaboration across a multidisciplinary team of care providers as well as adequate knowledge and education on the part both of PwD and HCPs.
The comprehensive education of HCPs is a key element underpinning the delivery of high-quality diabetes care. Primary care professionals (PCPs) play a particularly crucial role in diabetes prevention and care as they represent the first point of contact for PwD. Not only do they manage the care of the vast majority of people living with T2D but they are also ideally placed to identify people at risk of developing the condition and provide them with the right treatment at the right time according to the latest evidence-based recommendations on diabetes care. Despite this, several barriers often prevent PCPs from translating scientific evidence into practice. These include, for example, lack of time, competing priorities, lack of familiarity with new treatments and misperceptions about PwD’s adherence to treatment. With about half the PwD not achieving their targets, fostering timely access to the right treatment is crucial to enable the prevention of diabetes-related complications and help PwD achieve the best possible quality of life.
HCPs education should be strengthened to reflect the need for equipping them with the right tools to implement the latest diabetes treatment guidelines, tackle clinical inertia and ultimately lower the risk for PwD of developing life-altering complications.
The comprehensive education of HCPs should also enable them in establishing a positive relationship with PwD, as this is a key driver of health outcomes, and PwD empowerment. HCPs should actively engage in shared decision-making and make PwD integral partners in their care journey. PwD should receive accessible information about their treatment to optimally manage their condition on a daily basis. They should feel free to ask questions and should not fear judgement. For HCPs, it is crucial to actively listen to PwD’s perspectives, taking into account their unique circumstances and recognising the type of support they require including, for example, the need for psychological support.
Fostering the adoption of digital health and strengthening the role of diabetes specialist nurses to tackle HCPs shortages
The need to strengthen HCPs’ education to adequately support PwD in achieving optimal health outcomes goes hand in hand with the urgent need to address the current shortage of healthcare workers. By 2030, the World Health Organization (WHO) projects a global deficit of 10 million healthcare workers. This shortage has significant implications for diabetes care.
Given the key role of PCPs and that of the other care workers who are integral part of the multidisciplinary teams supporting PwD, an under-resourced, underfunded and understaffed primary care system is a major obstacle to the effective prevention, management and treatment of diabetes and contributes directly to a care deficit and higher disease burden for PwD.
Currently, one third of PwD are undiagnosed. The lack of staff at the primary care level negatively affects PCPs’ ability to diagnose PwD and identify people at risk of developing the condition. Once diagnosed, PwD require regular routine checks and screening for complications as well as structured education and support from care workers to be able to make informed decisions and optimally manage their condition on a daily basis. Understaffing can undermine the ability of health systems to conduct regular checks for all PwD. In England, for example, it is estimated that, in 2021-22, less than half of PwD received all the required checks.
Diabetes specialist nurses (DSNs) play a key role in diabetes prevention, management and care. They are often tasked with educating PwD on self-management techniques and lifestyle changes, and generally supporting them in their journey. Despite this, they often do not receive specialised academic training in diabetes and, in most countries, are not allowed to prescribe medications. DSNs’ role, availability and workload are also inevitably affected by the current healthcare workforce shortage. According to WHO, the Europe Region has on average 80 nurses per 10,000 people. Strengthening their role by investing in nursing education and infrastructure would not only benefit the health outcomes of PwD, but it would also help shore up the resilience of health systems by improving the effectiveness of diabetes prevention, management and care.
Fostering the adoption of digital health solutions can also help free up human and financial resources for health systems and help tackle the shortage of HCPs while facilitating the delivery of high-quality care. By leveraging the use of data and AI, innovative care delivery models can support the deployment of integrated and personalised care, improve the quality of the interaction between HCPs and PwD, and inform more effective diabetes prevention strategies.
In the lead up to World Diabetes Day, let’s raise awareness of the need to accelerate action towards improving HCPs education and overcome the shortfall in healthcare workforce by investing in primary care, strengthening the role of DSNs and fostering the adoption of digital solutions to improve health systems’ resilience. Together, United, Let’s Act on Diabetes

Nothing about us, without us
Diabetes is a hugely complex disease which requires 24/7 management. PwD need to make constant decisions regarding food, physical activity, and medication, often with limited input from healthcare professionals (HCPs). For PwD, even normal activities such as going for walks, eating an ice-cream, travelling or breastfeeding a baby, require extra thought and planning. Empowerment and engagement of people living with diabetes (PwD) are pivotal to enable them to manage their diabetes effectively and improve overall well-being. Empowered PwD are better equipped to become active partners in their care, set prioritiesand make informed decisions.
According to the World Health Organization (WHO), patient empowerment is the process by which individuals gain control over decisions and actions affecting their health. This empowerment extends from the individual level to the community level, encompassing various aspects of self-care and advocacy. As well as ensuring that PwD are better equipped to manage their care, engagement and empowerment must cover all other aspects, affecting them.
Engagement and empowerment must extend to everything that affects PwD
PwD’s meaningful engagement and participation in research, for example, is essential to ensure that new innovations in diabetes care address their unmet medical needs and reflect their perspectives and preferences. This engagement – be it in the definition of research needs or design of clinical trials, coupled with engagement in evaluation processes as well as approval and reimbursement decisions – should be seen as a key driver in shaping the future of diabetes care.
Several strategies can be leveraged to promote empowerment
Obstacles to PwD empowerment are diverse, including health literacy, socio-economic factors, healthcare system integration, and insufficient recognition of the importance of citizen participation. However, several strategies can, and should, be leveraged to promote empowerment.
The provision of structured diabetes education and peer support programmes: this provides PwD with access to information, understanding of their condition, knowledge of the healthcare system as well emotional support.
HCP awareness-raising and education: HCPs play a vital role in facilitating PwD empowerment. When HCPs are aware of its importance, they can build collaborative relationships.
Language matters: all communication must be clear and respectful, free from jargon and blame, and explained in a way allowing for full participation.
Governance: across the board, governance frameworks need to be designed to embed citizen participation to the same level as that of other stakeholders.
In the lead up to World Diabetes Day we call for increased engagement and empowerment of PwD to ensure optimal health outcomes and the best possible quality of life. Together, United, Let’s Act on Diabetes.

Advancing research and innovation in diabetes: a century of progress and the road ahead
One hundred years ago, the discovery of insulin revolutionised diabetes care. Since then, an accelerating number of innovations has emerged, from new medicines, to devices, technologies and digital solutions that improve diabetes management and treatment and reduce the burden of the condition on people living with diabetes (PwD). These include, for example, novel approaches to the delivery of care supported by digital tools such as web portals, apps, telemedicine, digital education services and digital therapeutics that can enhance diabetes management, interactions with HCPs, access to knowledge and information, peer support and PwD empowerment.
However, despite these significant advances, unmet medical needs remain. Diabetes prevalence continues to rise, one in two PwD do not meet their blood glucose targets and many of them develop diabetes-related complications. Required advances include those supporting more effective and targeted diabetes treatment and prevention as well as those enabling an improvement in the quality of life and health outcomes that existing solutions do not currently offer, and ultimately the possibility of a cure.
Some of the promising research areas span cell replacement therapies that could restore the body’s ability to produce insulin. Others include new sensors and long-term implantable devices for diabetes management and new insulin delivery mechanisms that can ease self-management and its burden for PwD.
More research and investments are also needed to improve the identification of those at risk of developing diabetes and its complications, address the side effects of existing treatment, optimise interventions aimed at preventing both type 1 and type 2 diabetes, address the interplay of diabetes with other conditions such as cardiovascular diseases and kidney disease and improve the understanding of the interactions between different medicines. Ultimately, extensive research is still needed to find a cure for diabetes. In this respect, a major recent breakthrough is a new drug that can delay the onset of type 1 diabetes in some individuals by an average of two years.
The transformative role of healthcare systems’ digitalisation in diabetes care
The digitalisation of healthcare systems, coupled with an increased use of data, new technologies, data analytics and AI, plays an essential role in the potential improvement in diabetes prevention, management and care.
Digitalisation can support the delivery of more personalised care by enabling the collection and analysis of data that advance our knowledge of diabetes and can be used to tailor treatments to PwD’s needs and preferences. It supports remote monitoring and self-management and facilitates shared decision-making between HCPs and PwD. It can also aid in the evaluation of health systems’ performance and improve the effective allocation of resources by leveraging data-driven insights.
Unlocking the full potential of health systems’ digitalisation requires the setup of frameworks that can support the use of novel tools and practices and scale up their adoption. In this context, initiatives such as the European Health Data Space can create a harmonised EU-wide data framework that could enable major breakthroughs in prevention and care while decreasing the cost of diabetes-related healthcare expenditure, freeing up health system resources and improving health systems resilience and sustainability.
In the lead up to World Diabetes Day, let’s raise awareness of the need to accelerate action on research and innovation to improve diabetes prevention, management and care and stimulate the digitalisation of healthcare systems. Together, United, Let’s Act on Diabetes.
A Call to Action for Diabetes Care and Universal Health Coverage
As stated by the WHO Constitution, “The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition”. With the adoption of the 2030 Agenda for Sustainable Development, world leaders have committed to ensuring access to Universal Health Coverage (UHC) for everyone by 2030. Strengthening healthcare systems and improving access to healthcare services as well as to medicines and technologies for people living with, or at risk of, developing diabetes is essential to achieve UHC.
Tackling inequalities to improve health outcomes and quality of life for PwD
Diabetes is a hugely complex condition that can affect every organ system in the human body and which requires 24/7 management on the part of people living with it. To be able to optimally manage their condition, prevent the development of life-altering complications and achieve the best possible quality of life, all people living with diabetes (PwD) need access to early diagnosis and to the right treatment at the right time. This includes uninterrupted and affordable access to medicines, technologies, supplies, tools and technologies as well as the provision of self-management education and psychological support and adequate screening for complications. Today, great inequalities persist in access to health services for PwD within and between European countries as well as in medicines and technologies, resulting in an elevated risk for them of developing diabetes-related complications and a shortened life expectancy.
Barriers to adequate access are numerous. Access to early diagnosis and to the right treatment at the right time and place as well as regular reassessments and screening for complications are, for example, often adversely affected by the current shortage of healthcare professionals (HCPs). Improving early action requires strengthening primary care systems and allocating resources more efficiently.
Another issue relates to the availability of medicines and technologies. In some countries, new diabetes medicines and technologies only become available months after they have reached PwD in other European countries. In other cases, access is limited to people with some types of diabetes or belonging to a specific age group, or supplies are provided in insufficient amounts. All too often, access to the medicines and technologies required for diabetes management is also restricted to those who are able to afford them.
The provision of structured diabetes education at the time of diagnosis and throughout the life course is also strongly related to the ability of PwD to optimally self-manage. And again, this is all too often lacking.
As a life-long condition, the type of health services and support PwD require access to may vary throughout their life course. The provision of integrated and person-centred care is essential to ensure that during the transition between stages of life, PwD maintain uninterrupted access to the medicines, devices, technologies and health services they require.
Diabetes care is a maker of healthcare systems’ resilience
Lately, existing inequalities in access to diabetes care have been exacerbated by the “permacrisis”, exemplified by the COVID-19 pandemic and other emergencies including wars and natural disasters. These events have further highlighted how the level of preparedness of governments, health systems and communities in responding to the need of PwD and ensuring uninterrupted access to care during emergencies, is often inadequate and how PwD are often disproportionately impacted by them. The COVID-19 pandemic in particular illustrated that the quality of diabetes prevention, management and care, which touch on all aspects of health systems, is a clear marker of their resilience, benefiting not just PwD and people living with other chronic conditions but also other citizens.
Strengthening healthcare systems and improving access to healthcare services for people living with, or at risk of, developing diabetes is therefore an essential step to achieve UHC. Improving diabetes prevention, management and care requires acting on several areas including,
- reaffirming political commitments on diabetes, increasing collaboration between stakeholders and improving the allocation of resources;
- understanding and acting on the social determinants of health and fostering the development of health-enabling environments;
- adopting integrated, person-centred and novel care pathways;
- providing comprehensive education to HCPs and ensuring adequate staffing levels;
- empowering PwD to be full partners in their own care and to engage in advocacy and research initiatives;
- and advancing new research and innovation in diabetes by leveraging the potential of digitalisation and the use of data.
In the lead up to World Diabetes Day, let’s raise awareness of the need to accelerate action on ensuring uninterrupted, equitable and affordable access to medicines, technologies and care to all PwD to reduce inequalities in health outcomes among European citizens and achieve UHC. Together, United, Let’s Act on Diabetes.
We wish to thank the “BI and Lilly Alliance” and Novo Nordisk for their support to IDF Europe World Diabetes Day initiatives
 |
 |
 |



